Abstract
Immune thrombocytopenia (ITP) is an autoimmune hemorrhagic disorder. Loss of peripheral immune tolerance in ITP patients leads to autoreactive T cells proliferation and production of auto-antibodies against platelet cell surface antigen. It was reported that the homeostasis of CD4+ T-cell subsets, including the balance of T helper1(Th1)/T helper2(Th2) and T helper17(Th17)/CD4+CD25+FOXP3+ regulatory T cells (Tregs), was disturbed in ITP patients.
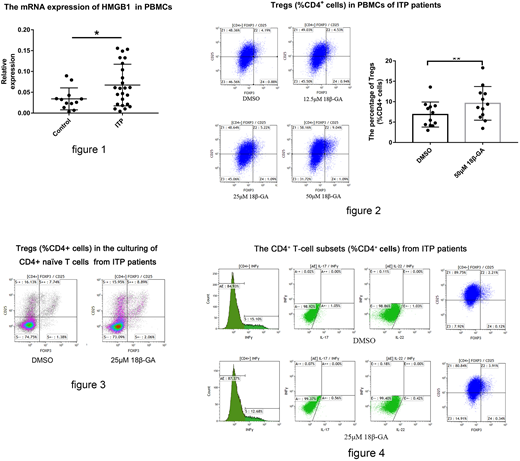
High-mobility group box 1 (HMGB1), a non-histone nuclear protein, plays a critical role not only inside of the cell as a DNA chaperone, but also outside of the cell as the damage associated molecular pattern molecule (DAMP). In our previous studies, we found a significant increase of HMGB1 expression in peripheral blood mononuclear cells (PBMCs) and blood plasma in ITP patients compared with healthy controls by q-PCR and ELISA analysis. (Fig. 1)
18β-glycyrrhetinic acid (18β-GA) is a novel pharmacological inhibitor of HMGB1 cytokine activities, which attributed effects like antioxidant, anti-viral, and anti-cancer activities, clinically used for the treatment of allergic purpura, chronic urticaria, ulcerative colitis possibly by upregulating Tregs. However, whether 18β-GA could regulate the immune homeostasis in ITP is unknown.
To examine whether 18β-GA could facilitate the development and function of Tregs in ITP, PBMCs were separated from ITP patients and healthy controls, and cultured with DMSO or different doses of 18β-GA (12.5μM/25μM/50μM/100μM). We observed a dose-dependent increase in the number of Tregs both in the culturing of PBMCs from ITP patients and healthy controls by flow cytometric analysis. (Fig. 2) And 18β-GA could significantly induce the apoptosis of PBMCs at high doses (50μM and 100μM), so we selected 25μM as the optimal dose in our in vitro study. In addition, we isolated the CD4+ naïve T cells to investigate whether 18β-GA could directly induce the development of Tregs. It was shown that 18β-GA could directly activate and induce the differentiation of Tregs from CD4+ naïve T cells. (Fig. 3)
Furthermore, we isolated the CD4+CD25+FOXP3+ Tregs from ITP patients, and then cocultured with CD4+CD25- effector T cells from the same patient at a ratio of 1:4, with the administration of 25μM 18β-GA or DMSO, and stimulated with anti-CD3 antibodies, anti-CD28 antibodies, and rhIL-2. After incubation for 5 days, the proliferation of effector T cells was analyzed by flow cytometry. The results showed that Tregs significantly inhibited the proliferation of effector T cells, and the addition of 18β-GA could enhance the suppressive effect of Tregs.
To survey whether 18β-GA could modulate the homeostasis of the CD4+ T-cell subsets and to explore the mechanism, we isolated the CD4+ T cells from ITP patients and cultured with 25μM 18β-GA or recombinant HMGB1 (rHMGB1) for 5 days. The levels of Th1, Th17 and Th22 showed significant decreases and the level of Tregs increased in the 18β-GA group, compared with the DMSO group by flow cytometry. (Fig. 4) However, this change was apparently attenuated in the rHMGB1 group. After incubation for 5 days, the culture supernatants were analyzed by ELISA, and the cells were used for analyses by q-PCR. We also observed a decrease in the level of HMGB1 expression from results of ELISA and q-PCR in the 18β-GA group, and the de-phosphorylation of NF-κB on the downstream pathway of HMGB1, as well as the decrease of mRNA levels of cytokines such as IL-1β, IL-6, and TNFα. We confirmed that 18β-GA could directly affect CD4+ T cells and modulate Th1/Th17/Th22/Tregs homeostasis by reducing the expression of HMGB1.
Finally, we established a passive murine model of ITP by injecting anti-CD41 antibody every 36 hours and divided ITP mice randomly into two groups with intraperitoneal injection of 18β-GA or the same dose of phosphate buffered saline as a control group. After 7 days, we examined the expression of Tregs by flow cytometry. It was observed that 18β-GA increased the numbers of Tregs in the peripheral blood, lymph nodes and spleen, compared with the control group.
Our findings demonstrated the regulatory role of 18β-GA in maintaining CD4+ T cells homeostasis in immune thrombocytopenia. 18β-GA could reduce the pro-inflammatory Th1, Th17 and Th22 cells whereas enhance the number and functions of Tregs by reducing the expression of HMGB1. Therefore, 18β-GA might be a promising therapeutic strategy for the management of ITP patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.